 This morning we attended the Allogeneic Pre-Transplant Class at Moffitt. It was our first time in the transplant inpatient unit as the class was held in 4W (fourth floor of the Moffitt inpatient area, west wing). Transplant inpatients are located on the third and fourth floors providing 18 private rooms per floor. Transplant patients, who require additional hospitalization due to post-transplant issues, use these same rooms unless the issues are life-threatening and the patient requires ICU.
This morning we attended the Allogeneic Pre-Transplant Class at Moffitt. It was our first time in the transplant inpatient unit as the class was held in 4W (fourth floor of the Moffitt inpatient area, west wing). Transplant inpatients are located on the third and fourth floors providing 18 private rooms per floor. Transplant patients, who require additional hospitalization due to post-transplant issues, use these same rooms unless the issues are life-threatening and the patient requires ICU.
Today’s class started with a diet technician. She provided nutrition guidelines for transplant patients. She mostly covered the details of the immunosuppressed diet. Dad will remain on the immunosuppressed diet from as short as a few months to much longer…over a year. Dad has always been fairly germaphobic. This trait may serve him well post-transplant and reduce his risk of infection.
After the transplant, Dad’s neutrophil count must be >500 to be discharged.
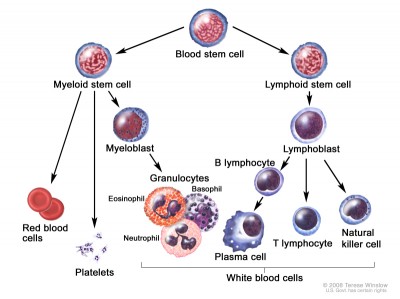
Next, Michele Stratton, RN, BMTCN, went over many aspects of the pre-transplant process. She started with the basics of what a stem cell is. A key measure to watch, after the transplant has occurred, is the neutrophil count. The count must be 500 before Dad will be discharged. He will have blood drawn everyday between 3:00am and 5:00am each morning.
I appreciated learning about the donor stem cell collection process. What a blessing stem cell donors are! They are truly saving lives. If you are between 18 and 44, give consideration to becoming a donor.
Yesterday, I mentioned in my post about the conditioning chemotherapy given just prior to the transplant. Michele spoke about the side effects of some of the chemotherapy drugs. The worst of the conditioning therapy side effects usually occur at Day +8, Day +9, and Day +10. They include the typical list of nausea and vomiting, diarrhea, decreased appetite, mucositis, hair loss, fatigue, changes in memory and concentration, decreased blood cell counts, and infection.

55 MS Powerpoint slides from today’s class.
Melphalan is one of the two chemotherapy drugs Dad is to receive. Unfortunately for Dad, Melphalan is one drug that produces mucositis (mouth sores). Dad experienced severe mucositis when he was being treated with Folotyn this summer. He was in terrible pain and unable to eat. Dad was so miserable he required prescription pain medication. I remember bringing him lots of milkshakes, which he could drink with a straw. The straw helped bypass the sores in his mouth. Michele stated that cryotherapy right before, during, and after the Melphalan infusion could help reduce the mucositis side effect. The cryotherapy is simple in concept but harder to execute. Dad will need to hold ice chips in his mouth for about 45 minutes. This does not mean simply chewing on some ice chips, but rather holding the chips on his tongue, continuously, for the 45 minutes. The ice will cause the blood vessels in his mouth to constrict and reduce the amount of Melphalan impacting his mouth.
On Day 0, when the stem cells are infused, Dad may receive pre-medications to prevent reactions to the donor’s stem cells. Pre-medications are driven by how much of a match the donor is and blood type, The closer the match the less pre-medications. We need to find out how close of a match Dad’s donor is.
Dad is not looking forward to being in the hospital for 3 to 3.5 weeks. Michele suggested items Dad should consider having in his room while he is an inpatient. She discouraged long, complex novels since most patients experience a change in concentration as a chemotherapy side effect. Additional items we are considering:
- Bose or Beats wireless speaker (Dad can play music from his iPhone)
- Apple TV (Dad can binge watch shows)
- Skull cap/beanie (Grandson can pick Dad out a few nice Nike and Under Armour skull caps)
Graft-versus-host-disease (GvHD) was discussed at length. Dad’s doctors are counting on some amount of graft-versus-tumor to eliminate any residual cancer. Thus, a little bit of GvHD is beneficial, but mostly it is not. Acute GvHD occurs within the first 100 days after the transplant. Chronic GvHD generally occurs within the first two years after the transplant.
Dad doesn’t have any Moffitt appointments for the remainder of the week. He deserves this short break before he starts radiation on Monday.

Thank you so much for sharing your dad’s story. With this disease being so rare, it is easy to feel alone on this journey. My wife has Mycosis Fungoides with some Sezary cell involvement. She is currently receiving Romedepsin therapy and seeing response to the drug. As stem cell transplant is one of the possible treatments down the road, I will be reading your posts with interest.
Thanks again for sharing.