by Jena | Mar 14, 2016 | Brentuximab Vedotin, Infectious Disease, Stem Cell Transplant |
Monday, March 14th at 2:00 p.m., Dad had his follow-up appointment with Dr. Ayala at the main campus of the Moffitt Cancer Center. The appointment started with Denise, transplant nurse, reviewing Dad’s current medications. She also asked about Dad’s current symptoms. Denise noted that Dad’s last blood transfusion was two days ago on Saturday.
Dad immediately asked Denise if she had a new transplant admission date. She did not. Denise said that Dr. Ayala had not allowed her to schedule the donor until he saw Dad. Denise anticipated Dr. Ayala would now allow her set a new admission date with the donor based upon what she was seeing and hearing during the appointment. She sought to manage Mom and Dad’s expectations by saying that the admission date would likely be at least seven days out. Dad expressed disappointment with the week long wait. According to Denise, it is common courtesy to provide the donor time to make plans to accommodate the transplant date. Denise also shared that Dr. Ayala had reached out to Dr. Sokol, hematology oncology, asking if Dad needs another dose of Brentuximab Vedotin.
At 2:45 p.m., Dr. Ayala came in and asked how Dad was feeling. Dad’s biggest complaint was in regards to his feet and legs due to their over radiation. They burn, tingle and randomly go numb. Dr. Ayala inquired of his appetite and his fitness. Dad has been going to the fitness center, exercising in a mask and gloves, every few days. Dad spends 20 minutes on the bike and does some free weights. I imagine that Dad has no problem getting on a bike nor accessing the weights. Others, in the fitness center, probably scurry away thinking Dad has some highly infectious disease when they see him wearing his mask and gloves. A perk of being immunosuppressed.
Dr. Ayala conducted a physical examination of Dad. The egg, which now looks like a black mushroom, on Dad’s head is starting to reduce in size. Dad calls it a “head decoration.” Dr. Ayala said that Dad’s skin looked perfect. Dr. Ayala checked Dad’s lungs, legs and feet. At the end of the physical exam, Dr. Ayala asked jokingly, “What are we going to do with you?”
Dr. Ayala observed that Dad has gotten weaker. Dr. Ayala said that he doesn’t have a solid reason not to proceed with the stem cell transplant. He stated that without a transplant, Dad has no chance for survival. Dr. Ayala increased the risk of Dad dying from the transplant to 30-40%. Dr. Ayala predicted that it will be a bumpy road, and it may not work.
Dad wanted to know about the status of his disease. Dr. Ayala said that Dad still has CTCL. It is well under control, but no for a long time. It will come back and in full force. From a CTCL point of view, Dad looked “beautiful.” Disease control was excellent. His blood and skin had cleared.
Mom inquired about Dad’s weight loss. We reviewed the trends displayed in Dad’s weight graph on the exam room computer. Since January, Dad has lost 14 pounds. Dr. Ayala instructed Dad to continue going to the gym, walk, get stronger, be cautious about infections, eat, and fatten up.
Dr. Ayala recommended that Dad not do another round of Brentuximab Vedotin since they are targeting an admission date of a week or less.
 Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until
Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until
Dad’s new admission date for transplant.
Dr. Ayala and Denise will determine the proper Bactrim dosage (the script says one amount and the medicine bottle says another). Denise will notify Dad about the donor and the confirmed admission date. Denise will develop and send Mom a new, custom calendar containing Dad’s key activities during the transplant.
Hopefully, the fourth time is a charm!
by Jena | Mar 13, 2016 | Brentuximab Vedotin, Infectious Disease |
Picking up on Monday, February 29th
8:20 a.m. Mom and I arrived at Moffitt. Dad had trouble getting and staying asleep due to his feet bothering him from the radiation treatment in January. Hunter, Dad’s Sunday night nurse, had given Dad pain medication.
Dorothie, Dad’s day nurse, said that blood had been ordered since Dad’s hemoglobin level was 6.6. They were waiting on the blood to arrive. The search was taking longer due the presence of antibodies in his blood.

Dad’s incentive spirometer.
8:48 a.m.
Karla Adams, transplant physician assistant, and Eleni, transplant physician assistant student, came to see Dad. They inquired how Dad was feeling.
- No chest pain. Dad had experienced a some PACs (premature atrial contractions) yesterday.
- Dad had received oxygen during the evening. Eleni and Karla checked Dad’s breathing and heart rate.
- His temperature had been doing well, staying under 100.
- Dad’s sodium had been a little low. Karla told Dad to drink Gatorade and even soda. He should eat pretzels and chips.
- Bactrim suppresses his blood count. It is being given for Dad’s PJP.
Karla was moving his follow-up CT scan from the main campus to the Moffitt Cancer Center at International Plaza (MIP), which was scheduled for March 9th. Karla was going to ask Dr. Ayala whether or not Dad should get his next brentuximab vedotin treatment on March 7th. Karla thought it may not be a good idea to get brentuxmiab vedotin while having an infection. Dad’s appointment with Dr. Baluch, infectious disease, was scheduled for March 10th at 7:30 a.m.
12:48 p.m.
Dr. Walsh and another from pulmonary came to visit. They asked Dad how he had been eating and drinking. Had he been coughing? They checked his breathing. They said to continue the course of treatment for the PJP. They will be monitoring the cultures from the BAL (bronchoalveolar lavage) procedure every day to see if anything else grows.
1:30 p.m.
Dad received magnesium via IV.
2:48 p.m.
Kristen, transition nurse, came to visit. She confirmed tomorrow’s MIP appt at 7:30 a.m. for labs and neupogen. These appointments would reoccur until meeting with Dr. Baluch and Dr. Ayala on March 10th.

Dad’s inpatient meal.
Later in the afternoon, Dad experienced another fever (100.8) with chills. This resulted in his discharge being canceled. Dad would stay another night.
Another night, another Moffitt meal.
March 1st
In the morning, Dad was feeling well. His temperature experience yesterday prior to discharge was not sustained. Dad continued to receive blood support until his successful discharge in the afternoon.
by Jena | Feb 28, 2016 | Brentuximab Vedotin, Campath (alemtuzumab), Infectious Disease, Radiation Therapy, Stem Cell Transplant |
Friday evening, February 26
 Since Dad was admitted very early Thursday morning, Dad’s oxygen saturation has been continuously monitored with a pulse oximeter on his fingertip. On Friday evening, his saturation level dropped enough to warrant oxygen supplementation. Mom stayed overnight with Dad in his room.
Since Dad was admitted very early Thursday morning, Dad’s oxygen saturation has been continuously monitored with a pulse oximeter on his fingertip. On Friday evening, his saturation level dropped enough to warrant oxygen supplementation. Mom stayed overnight with Dad in his room.
Saturday, February 27
Dad’s temperature was up and down throughout the day. A couple of times Dad experienced a fever that included chills and uncontrollable shivering. He continued to be on oxygen. Dad didn’t have much of an appetite and wouldn’t eat the Moffitt food.
Dr. Ayala, transplant doctor, visited Dad. Mom put me on speakerphone so that I could participate. Dr. Ayala had conferred with Dr. Velez, infectious disease. Dr. Ayala restated what we had heard from Dr. Velez on Friday afternoon. Dr. Ayala wanted Dad to stay another night due to his fever and chills. I inquired about the donor. Dr. Ayala said that the donor was willing to wait for Dad. Hallelujah! Dad is extremely blessed to have such a donor.
I believe the doctors attribute Dad’s bone marrow aplasia from his Campath (alemtuzumab) treatments. Campath is a monoclonal antibody directed against CD52, an antigen (marker) found on both B and T lymphocytes. The drug is used most often to treat chronic lymphocytic leukemia and has been used in the treatment of advanced CTCL. Mom has always questioned if Dad received too many Campath treatments and wondered why Dad wasn’t more closely monitored for bone marrow aplasia.
Dr. Ayala said that Dad is in a difficult position. He has fungal pneumonia because he essentially has no immune system. The only way to get a new immune system is to have a stem cell transplant. Dad must get well in order to receive the stem cell transplant. Dr. Ayala spoke in a way that he was not confident that Dad would be able receive a stem cell transplant in the future.
 In the afternoon, Daughter and I went to visit Mom and Dad to bring some additional clean clothes for Mom and Dad since Dad was going to remain in the hospital. We also came bearing Chick-fil-A. Nuggets had to be more appealing than the flavorless Moffit food. Upon our arrival, Dad was extremely happy to see us and was slightly overcome with emotion. Perhaps it was the thrill of receiving Chick-fil-A! We could tell that he was quite uncomfortable and not his smiling, happy self. His eyes were dull and fatigued. He seemed physically agitated. Daughter and I were not expecting to see him this way. I sought out Dad’s nurse, Tammy, to give him something to take the edge off.
In the afternoon, Daughter and I went to visit Mom and Dad to bring some additional clean clothes for Mom and Dad since Dad was going to remain in the hospital. We also came bearing Chick-fil-A. Nuggets had to be more appealing than the flavorless Moffit food. Upon our arrival, Dad was extremely happy to see us and was slightly overcome with emotion. Perhaps it was the thrill of receiving Chick-fil-A! We could tell that he was quite uncomfortable and not his smiling, happy self. His eyes were dull and fatigued. He seemed physically agitated. Daughter and I were not expecting to see him this way. I sought out Dad’s nurse, Tammy, to give him something to take the edge off.
Since Dr. Ayala told Dad that he must get out of bed and walk, Mom now had a mission. Later in the evening, she had Dad up and moving around a bit. Dad ate dinner sitting in the chair.
Sunday, February 28
Dad was more lively today. Could it be the Chick-fil-A? He was sitting in the chair. Mom had plans for him to walk “laps” on the third floor of the Blood & Marrow Transplant (BMT) unit. At 12:37 p.m., Dr. Ayala and Karla, transplant physician assistant, came to visit Dad. Dr. Ayala listened to Dad’s lungs and checked his mouth and throat. Dr. Ayala found Dad’s throat to be clear and stated that it was much better. Dad hasn’t experienced any fever today. Dr. Ayala said that Dad looked better overall, especially as compared to yesterday. Dad is to remain at Moffitt tonight since Dr. Ayala wants to be cautious. Dad will be setup to be discharged earlier tomorrow. Dad will continue his antibiotics and anti-fungal medications.
Dr. Ayala did say that this fungal pneumonia was a major setback and that he cannot predict the future. He said that we will see if Dad is able to move forward with the stem cell transplant. Dr. Ayala sounded quite noncommittal. I don’t think Mom heard Dr. Ayala, yesterday, state the he was not confident about Dad’s ability to get a stem cell transplant in the future. Mom seemed surprised by Dr. Ayala’s statement today.
Mom inquired about the slow healing, necrotic egg on Dad’s head that now looks like a big, black mushroom. She wanted to know if it may contain fungus. Dr. Ayala said that it does not, because if it did, Dad would be experiencing pain and soreness at the site. Dr. Ayala doesn’t want to tamper with it as he believe it is healing. He said that the radiation therapy worked marvelously on Dad’s tumors including the egg. The plan is for Dad to see Dr. Baluch, infectious disease, and Dr. Ayala in a couple weeks in the BMT clinic. They will discuss another brentuximab vedotin treatment for Dad.
Before leaving the room, Dr. Ayala told Dad to go for a walk, and Karla said Dad would be receiving a platelet transfusion later today.
by Jena | Feb 4, 2016 | Brentuximab Vedotin, Radiation Therapy, Stem Cell Transplant |
Upon arrival to the Moffitt Cancer Center this morning, I went straight to Starbucks on the first floor. As I stood in line to order my standard venti-skinny-vanilla latte and Mom’s tall-hazelnut latte, Krista, hematology oncology PA, greeted me with a hug…a real hug… long, tight, and meaningful. Krista is always a bundle of energy and full of smiles. She immediately inquired about Dad. I actually think she was a bit puzzled to see me at the Starbucks. She probably had assumed that I would be at the inpatient section of Moffitt with Dad in the Blood & Marrow Transplant unit. Krista hadn’t heard that Dad’s transplant had been canceled. Once I brought Krista up to speed, she gave me positive words of encouragement and wanted me to tell Mom and Dad “hello” and that she is thinking of them. Krista said that if anyone deserves the transplant…it is Dad. She also said she and Dr. Sokol miss Dad’s regular emails. I got a good laugh. Dad had smartly figured out the best way to communicate with Dr. Sokol and Krista was through email. With an iPhone constantly in Dad’s hands, Dad was often an emailing machine, communicating daily with Dr. Sokol and Krista. I teased Krista saying they were probably glad to get a break from Dad’s barrage of daily emails.
Upstairs, we first met with Denise, transplant coordinator. She wanted to review what had transpired since we met with her and Dr. Ayala last month. Dad described the radiation and brentuximab vedotin treatments. He recounted the blood and platelet transfusions he received along with the neupogen shots. Dr. Ayala came in and gave Dad a thorough physical examination of his tumors and skin. The tumors on Dad’s head are nicely reduced but black and scabby. Dr. Ayala noted that Dad had “active” borders on a couple of the tumors on his head. The subcutaneous golf-ball sized tumor, near the crook of Dad’s left arm, is now gone. Overall, Dr. Ayala was pleased with the results of the radiation and brentuximab vedotion treatments. He could not discern which of the treatments or both were having the positive impact. Dr. Ayala confirmed that Dad has reached his best opportunity for a stem cell transplant. Thus, Dad is moving forward with the younger donor…19 years old, living in Germany.
The updated schedule of events:
 February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs, flow cytometry to check the Sézary count)
February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs, flow cytometry to check the Sézary count)- February 15th: Receive third brentuximab vedotin infusion
- February 17th: Physical evaluation of the 19 year old donor
- February 18th: Follow-up visit with Dr. Ayala
- February 19th: Removal of PICC and placement of central line catheter
- February 20th: Flush the central line catheter
- February 21st: Admission for stem cell transplant
In an ironic way, I enjoy the doctor visits with Mom and Dad. One’s true character shows during difficult times. I am constantly amazed at the sustained strength both, Mom and Dad, exhibit. Their interactions with the medical staff are always upbeat and spirited. Lots of laughter, jokes, hugs, and gratitude are vividly on display during each visit. This is irregardless of who the medical staff are…from the most educated and experienced doctor to the new, fresh-out-of-school technician. If you were to walk by the exam room, you would not suspect that we are discussing cancer and the risk of death.
by Jena | Jan 25, 2016 | Brentuximab Vedotin, Radiation Therapy, Stem Cell Transplant |
Dad’s Monday started early with a blood draw at 7:30 a.m. at the Moffitt Cancer Center at International Plaza (MIP). He then met with Mark Honor, physician assistant, at 7:45 a.m. Dad’s platelets are down to 13. His white blood cell count is low at 0.4, but his hemoglobin is looking fair at 9.5. Looks like the two bags of blood last week helped boost his hemoglobin. Dr. Sokol, hematology oncology, indicated that Dad should receive 3 shots of neupogen this week, on Tuesday, Wednesday and Thursday, to increase his white blood cell count. At 9:30 a.m., Dad received his second infustion of brentuximab vedotin. During the first 30 minutes, Dad received his pre-medications of Tylenol and Benadryl. Dad then received the brentuximab vedotin for the next 30 minutes without any side effects. At 12:45 p.m., Dad received his 6th of 8 TSEB treatments. When he says that the TSEB treatments are “unpleasant,” I can tell he is biting his tongue from saying what he really thinks. Only two more rotisserie sessions left.
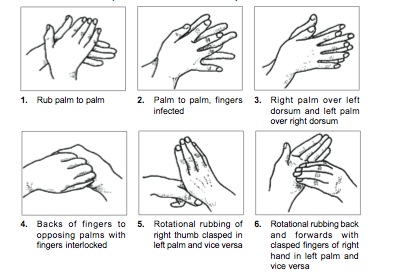
How to wash your hands.
I am already somewhat germaphobic (and claim that Dad passed that gene onto me), but with Dad’s weak immune system, I am constantly washing my hands. I am always barking at Husband, Son and Daughter to wash their hands. Today, Son stayed home from school due to a terrible cough. Mom is highly concerned that I will end up with the same terrible cough, which would impact my ability to be there next week for Dad’s move-in day. Dad will be admitted as an in-patient for his stem cell transplant next week on Thursday, February 4th.
Time for me to wash my hands.
by Jena | Jan 8, 2016 | Brentuximab Vedotin, Radiation Therapy, Stem Cell Transplant |
As another step in the pre-transplant testing phase, Dad started his day with 20 vials of blood drawn. The blood will be tested for additional organ functions and past exposure to diseases. Dad’s white blood cell count was lower today at 1.74. His hemoglobin is adequate at 8.5 due to his blood transfusion. The platelets are still low at 22. His platelet count will need to be 50 in order to get his central line catheter placed. Dad may need a platelet transfusion the day before his central line catheter procedure is done.
Next, we met with Denise, the transplant coordinator, and Dr. Ayala, the transplant doctor, for Dad’s re-evaluation visit. This purpose of the visit was to review the vital organ testing results and finalize the plan for transplant. Denise said that Dad was one Dr. Ayala’s three patients being seen this afternoon for the re-evaluation visit. Perhaps the three of them will be “neighbors” in the transplant unit for 20+ days.
Denise shared the news that one of the two matched donors is able to accommodate the new transplant date of February 9th. The donor is a 31 year old, European male. We were delighted to hear that Dad and his donor are a 10/10 match. I confirmed with Denise that the better Dad and donor are matched, the less chance for GvHD for Dad.
Dad’s CT scan showed minor sinusitis, some lymph node involvement and cutaneous lesions. Dad’s bone marrow biopsy resulted in a Sézary count of zero. Excellent! Dr. Ayala said that the chromosome analysis revealed an abnormal chromosome, an extra copy of chromosome 8. People usually only have two copies, one from each parent, of chromosome 8. This extra copy may be an indicator of myelodysplastic syndrome (MDS). Dr. Ayala said that the stem cell transplant should address the MDS. Both, Dad’s EKG and echo, were unremarkable and completely normal. Dr. Ayala was very impressed with Dad’s pulmonary function test. Dad must have some large capacity lungs.

Mom and Dad’s fitness center in their hometown in the Florida panhandle.
Denise remarked that Dad, at 75 years old, is in better shape than 50 year olds that they take to transplant. My parents have been the epitome of healthy. They would “move more, eat less.” Prior to Dad’s cancer, they worked out nearly everyday at their local fitness center. Mom was addicted to Zumba and would get cranky if she missed a class. Mom and Dad took zero prescription medications, which amazed any and all doctors they visited. Even at Moffitt, the doctors refer to Dad as very “healthy.” This seems like an oxymoron.
Dad would not have the opportunity of a stem cell transplant without being very healthy. Dr. Ayala said Dad will be the oldest CTCL stem cell transplant patient Moffitt has had. A key driver of this decision was that Dad is so healthy. Dad set a new goal to go to the gym in their condo once per day. You can imagine with all the treatments, side effects, and tumors that Dad has not been moving and working out as he had before cancer.
Together, Dad and Dr. Ayala signed several consent forms:
- One was consent for the drugs Fludarabine and Melphalan, which are planned for Dad’s conditioning therapy. The purpose of the conditioning therapy is to destroy the cancer cells in Dad’s body. The conditioning therapy starts on the first day Dad is admitted to the hospital, February 4th. In a prior post, I mentioned a Stanford Medicine article that spoke about different conditioning therapies Stanford has been studying for their CTCL stem cell transplant patients. I located a recent presentation of Dr. Youn Kim’s titled “Managing MF and SS with Allogeneic HSCT.” I asked about one conditioning therapy described, in Dr. Kim’s presentation, as a method to reduce GvHD. Dr. Ayala was kind and patient in addressing my inquiry and responding to the printed Stanford presentation slides I put before him on the desk. Dr. Ayala knew of the Stanford research done on that particular conditioning method. It had been published in The New England Journal of Medicine in 2005. He provided his view of the research and shared that Moffitt had a submitted a response to that study. In the end, Dr. Ayala said Dad was getting the best conditioning therapy for his personal situation and that the 2005 Stanford method was not for Dad.
- There were three consents to provide Dad’s data and a blood sample for research purposes within Moffitt and another external organization.
- The last consent was only for patients with European donors. It acknowledges that the European donor may pass Creutzfeldt-Jakob disease, aka Mad Cow disease, onto Dad. At this time there is no test used to identify donors who have Creutzfeldt-Jakob. In recent years, there have been blood and urine tests developed and studied as a reliable screening test. Unfortunately for now, doctors can only confirm the disease with a brain tissue sample. Dr. Ayala reassured Dad by saying that he has never heard of a single transmission of Mad Cow disease in the stem cell transplant community. Dr. Ayala said that it is a “theoretical” risk.
Between now and the admission date of February 4th, Dad continues his radiation therapy with Dr. Montejo. The last radiation treatment is scheduled for January 22nd. Dr. Sokol has squeezed in a second brentuximab vendotin infusion for January 25th.
 Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until
Denise will work with Mark, PA at Moffitt Cancer Center at International Plaza (MIP), to setup appointments for regular blood support and a daily line flush until


 Since Dad was admitted very early Thursday morning, Dad’s oxygen saturation has been continuously monitored with a pulse oximeter on his fingertip. On Friday evening, his saturation level dropped enough to warrant oxygen supplementation. Mom stayed overnight with Dad in his room.
Since Dad was admitted very early Thursday morning, Dad’s oxygen saturation has been continuously monitored with a pulse oximeter on his fingertip. On Friday evening, his saturation level dropped enough to warrant oxygen supplementation. Mom stayed overnight with Dad in his room. In the afternoon, Daughter and I went to visit Mom and Dad to bring some additional clean clothes for Mom and Dad since Dad was going to remain in the hospital. We also came bearing
In the afternoon, Daughter and I went to visit Mom and Dad to bring some additional clean clothes for Mom and Dad since Dad was going to remain in the hospital. We also came bearing  February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs,
February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs, 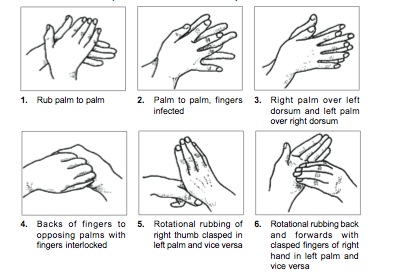

Recent Comments