
The pre-transplant train continues to move along its tracks. We met with Denise, the transplant coordinator, this morning. She shared that Dad has a tentative transplant admission date of February 4th and a transplant date of February 9th. Denise is awaiting confirmation from the two donors that one of them is available to donate according to this new proposed date. Denise reviewed the four consents that we will need to sign when we meet with Dr. Ayala, Dad’s transplant doctor, on January 8th.
One of the consents is for the two chemotherapy drugs to be administered starting Day -5 when Dad is admitted on February 4th. The two drugs are Fludarabine and Melphalan and seem to be the standard Moffitt transplant conditioning regimen. Last night, I ran across a recent article, “The rarest of rashes,” in the Stanford Medicine magazine, which describes how Stanford is now skipping the chemotherapy that has been considered a prerequisite to stem cell transplant for CTCL patients. Instead, the Stanford team is preparing each patient for transplant in a customized way by tailoring a combination of drugs and radiation that the Stanford team believes is most applicable to the patient’s disease. The goal of the customized approach is to reduce the spread of the disease as much as possible and eliminate skin tumors before transfusing the donor’s stem cells to eliminate any remaining disease in the patient. I inquired about the new Stanford method with both Denise, the transplant coordinator, and Karla, the transplant PA. Neither seemed to be familiar with this new Stanford method, but they did encourage me to ask Dr. Ayala when we meet with him next week.
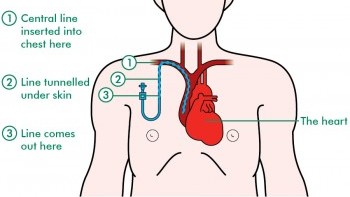
Central catheter line. Image from http://www.macmillan.org.uk/
On February 3rd, Dad will have his PICC (peripherally inserted central catheter) line removed and a central catheter line inserted. He will be sedated. A minimum platelet count of 50 (50,000) is required for the procedure. Denise, the transplant coordinator, believes that Dad may need a platelet transfusion prior to the procedure since his platelet count continues to be low. The central catheter line will remain until approximately 4- 6 weeks post transplant. The timing will be driven by Dad’s blood counts and ability to clot (platelets). At that time, the central catheter line will be removed, and a port will be inserted.
Denise indicated that there was no firm decision about brentuximab vedotin from the doctors. Karla believed that it may be used during post transplant. Thus, Dad sent an email to Dr. Sokol, malignant hematology, and Dr. Ayala, transplant, inquiring about using brentuximab vedotin as a systemic treatment.
One of the last topics discussed with Denise was graft versus host disease (GvHD). It is a condition that might occur after the transplant. Dad may experience acute GvHD and/or chronic GvHD. Denise described the symptoms of GvHD. One of the symptoms is a rash, which is also how CTCL appears. A skin punch biopsy would be done to determine if it is GvHD or the return of CTCL.
In the BMT Treatment Center, Dad received a blood transfusion today since his hemoglobin level had dropped from yesterday from 7.7 to 7.1. Only one unit today since Dad’s schedule was full with other appointments including more vital organ function testing (EKG and ECHO). Karla went ahead and scheduled Dad for a second unit tomorrow.

Trackbacks/Pingbacks