by Jena | Feb 18, 2016 | Stem Cell Transplant |
 Yesterday, Dad’s second donor, the 19 year old from Germany, was to have his physical evaluation to confirm that he is able to serve as a donor for the stem cell transplant. As of 9:45 p.m. last night, Dad still hadn’t heard. We are a bit frustrated since there has been no communication from Denise, the transplant coordinator, about the donor’s physical evaluation results and a “surprise” appointment for a bone marrow biopsy scheduled for today. Dad attempted to reach Denise via phone and email yesterday with no success.
Yesterday, Dad’s second donor, the 19 year old from Germany, was to have his physical evaluation to confirm that he is able to serve as a donor for the stem cell transplant. As of 9:45 p.m. last night, Dad still hadn’t heard. We are a bit frustrated since there has been no communication from Denise, the transplant coordinator, about the donor’s physical evaluation results and a “surprise” appointment for a bone marrow biopsy scheduled for today. Dad attempted to reach Denise via phone and email yesterday with no success.
Dad was scheduled to be at the main campus of the Moffitt Cancer Center at 7:15 a.m. for his bone marrow biopsy. I suggested to Dad that he refuse the procedure until he received confirmation directly from Denise. Dad has been under going some repeat pre-transplant testing since some of the prior tests had expired after 30 days, such as the CT scan of his sinuses and chest. There had not been a discussion about a repeat bone marrow biopsy. We don’t want Dad to repeat tests unnecessarily.
We should learn more later today as Dad is scheduled to meet with Dr. Ayala, transplant doctor, at 1:00 p.m. today.
by Jena | Feb 4, 2016 | Brentuximab Vedotin, Radiation Therapy, Stem Cell Transplant |
Upon arrival to the Moffitt Cancer Center this morning, I went straight to Starbucks on the first floor. As I stood in line to order my standard venti-skinny-vanilla latte and Mom’s tall-hazelnut latte, Krista, hematology oncology PA, greeted me with a hug…a real hug… long, tight, and meaningful. Krista is always a bundle of energy and full of smiles. She immediately inquired about Dad. I actually think she was a bit puzzled to see me at the Starbucks. She probably had assumed that I would be at the inpatient section of Moffitt with Dad in the Blood & Marrow Transplant unit. Krista hadn’t heard that Dad’s transplant had been canceled. Once I brought Krista up to speed, she gave me positive words of encouragement and wanted me to tell Mom and Dad “hello” and that she is thinking of them. Krista said that if anyone deserves the transplant…it is Dad. She also said she and Dr. Sokol miss Dad’s regular emails. I got a good laugh. Dad had smartly figured out the best way to communicate with Dr. Sokol and Krista was through email. With an iPhone constantly in Dad’s hands, Dad was often an emailing machine, communicating daily with Dr. Sokol and Krista. I teased Krista saying they were probably glad to get a break from Dad’s barrage of daily emails.
Upstairs, we first met with Denise, transplant coordinator. She wanted to review what had transpired since we met with her and Dr. Ayala last month. Dad described the radiation and brentuximab vedotin treatments. He recounted the blood and platelet transfusions he received along with the neupogen shots. Dr. Ayala came in and gave Dad a thorough physical examination of his tumors and skin. The tumors on Dad’s head are nicely reduced but black and scabby. Dr. Ayala noted that Dad had “active” borders on a couple of the tumors on his head. The subcutaneous golf-ball sized tumor, near the crook of Dad’s left arm, is now gone. Overall, Dr. Ayala was pleased with the results of the radiation and brentuximab vedotion treatments. He could not discern which of the treatments or both were having the positive impact. Dr. Ayala confirmed that Dad has reached his best opportunity for a stem cell transplant. Thus, Dad is moving forward with the younger donor…19 years old, living in Germany.
The updated schedule of events:
 February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs, flow cytometry to check the Sézary count)
February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs, flow cytometry to check the Sézary count)- February 15th: Receive third brentuximab vedotin infusion
- February 17th: Physical evaluation of the 19 year old donor
- February 18th: Follow-up visit with Dr. Ayala
- February 19th: Removal of PICC and placement of central line catheter
- February 20th: Flush the central line catheter
- February 21st: Admission for stem cell transplant
In an ironic way, I enjoy the doctor visits with Mom and Dad. One’s true character shows during difficult times. I am constantly amazed at the sustained strength both, Mom and Dad, exhibit. Their interactions with the medical staff are always upbeat and spirited. Lots of laughter, jokes, hugs, and gratitude are vividly on display during each visit. This is irregardless of who the medical staff are…from the most educated and experienced doctor to the new, fresh-out-of-school technician. If you were to walk by the exam room, you would not suspect that we are discussing cancer and the risk of death.
by Jena | Feb 3, 2016 | Stem Cell Transplant |
This is the week. Or so we thought. Plans were in place. Preparations were completed with anticipation that Dad would be admitted as an inpatient to Moffitt tomorrow. One of Dad’s key preparations was to get his 2015 taxes prepared and sent to his accountant. On Monday, while standing at the UPS counter to ship the tax paperwork to his accountant, Dad received a call from Denise, the transplant coordinator. Dad’s donor did not pass his physical evaluation. There would be no transplant at this time.
Rather than moving Dad into Moffitt tomorrow, we are meeting with Dr. Ayala, transplant doctor, to learn about next steps. I believe Denise is seeking the availability of Dad’s second “perfect match” donor. The second donor is a 19 year old male, who was unavailable the month of January and most of February.
 The timing of the radiation and systemic treatments Dad has just undergone in January was perfectly aligned for Dad to be admitted this week and receive the stem cells next week. Timing is crucial to increasing the chances of a positive outcome of the transplant. The goal is to have reduced the cancer in Dad’s blood and his skin, as much as possible, at the time the donor’s stem cells are transplanted to Dad.
The timing of the radiation and systemic treatments Dad has just undergone in January was perfectly aligned for Dad to be admitted this week and receive the stem cells next week. Timing is crucial to increasing the chances of a positive outcome of the transplant. The goal is to have reduced the cancer in Dad’s blood and his skin, as much as possible, at the time the donor’s stem cells are transplanted to Dad.
Dad is racing against the clock for a transplant. How quickly will Dad’s cancer come back? What treatments can Dad endure to sustain him until the second donor is available? How long must Dad wait? Is the second donor healthy enough to pass his physical evaluation, unlike the first donor? We shall see.
by Jena | Jan 25, 2016 | Brentuximab Vedotin, Radiation Therapy, Stem Cell Transplant |
Dad’s Monday started early with a blood draw at 7:30 a.m. at the Moffitt Cancer Center at International Plaza (MIP). He then met with Mark Honor, physician assistant, at 7:45 a.m. Dad’s platelets are down to 13. His white blood cell count is low at 0.4, but his hemoglobin is looking fair at 9.5. Looks like the two bags of blood last week helped boost his hemoglobin. Dr. Sokol, hematology oncology, indicated that Dad should receive 3 shots of neupogen this week, on Tuesday, Wednesday and Thursday, to increase his white blood cell count. At 9:30 a.m., Dad received his second infustion of brentuximab vedotin. During the first 30 minutes, Dad received his pre-medications of Tylenol and Benadryl. Dad then received the brentuximab vedotin for the next 30 minutes without any side effects. At 12:45 p.m., Dad received his 6th of 8 TSEB treatments. When he says that the TSEB treatments are “unpleasant,” I can tell he is biting his tongue from saying what he really thinks. Only two more rotisserie sessions left.
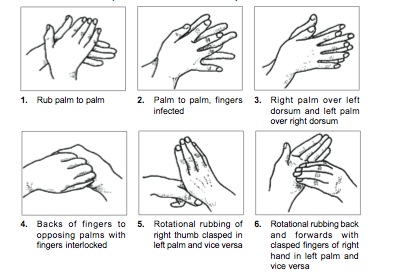
How to wash your hands.
I am already somewhat germaphobic (and claim that Dad passed that gene onto me), but with Dad’s weak immune system, I am constantly washing my hands. I am always barking at Husband, Son and Daughter to wash their hands. Today, Son stayed home from school due to a terrible cough. Mom is highly concerned that I will end up with the same terrible cough, which would impact my ability to be there next week for Dad’s move-in day. Dad will be admitted as an in-patient for his stem cell transplant next week on Thursday, February 4th.
Time for me to wash my hands.
by Jena | Jan 8, 2016 | Brentuximab Vedotin, Radiation Therapy, Stem Cell Transplant |
As another step in the pre-transplant testing phase, Dad started his day with 20 vials of blood drawn. The blood will be tested for additional organ functions and past exposure to diseases. Dad’s white blood cell count was lower today at 1.74. His hemoglobin is adequate at 8.5 due to his blood transfusion. The platelets are still low at 22. His platelet count will need to be 50 in order to get his central line catheter placed. Dad may need a platelet transfusion the day before his central line catheter procedure is done.
Next, we met with Denise, the transplant coordinator, and Dr. Ayala, the transplant doctor, for Dad’s re-evaluation visit. This purpose of the visit was to review the vital organ testing results and finalize the plan for transplant. Denise said that Dad was one Dr. Ayala’s three patients being seen this afternoon for the re-evaluation visit. Perhaps the three of them will be “neighbors” in the transplant unit for 20+ days.
Denise shared the news that one of the two matched donors is able to accommodate the new transplant date of February 9th. The donor is a 31 year old, European male. We were delighted to hear that Dad and his donor are a 10/10 match. I confirmed with Denise that the better Dad and donor are matched, the less chance for GvHD for Dad.
Dad’s CT scan showed minor sinusitis, some lymph node involvement and cutaneous lesions. Dad’s bone marrow biopsy resulted in a Sézary count of zero. Excellent! Dr. Ayala said that the chromosome analysis revealed an abnormal chromosome, an extra copy of chromosome 8. People usually only have two copies, one from each parent, of chromosome 8. This extra copy may be an indicator of myelodysplastic syndrome (MDS). Dr. Ayala said that the stem cell transplant should address the MDS. Both, Dad’s EKG and echo, were unremarkable and completely normal. Dr. Ayala was very impressed with Dad’s pulmonary function test. Dad must have some large capacity lungs.

Mom and Dad’s fitness center in their hometown in the Florida panhandle.
Denise remarked that Dad, at 75 years old, is in better shape than 50 year olds that they take to transplant. My parents have been the epitome of healthy. They would “move more, eat less.” Prior to Dad’s cancer, they worked out nearly everyday at their local fitness center. Mom was addicted to Zumba and would get cranky if she missed a class. Mom and Dad took zero prescription medications, which amazed any and all doctors they visited. Even at Moffitt, the doctors refer to Dad as very “healthy.” This seems like an oxymoron.
Dad would not have the opportunity of a stem cell transplant without being very healthy. Dr. Ayala said Dad will be the oldest CTCL stem cell transplant patient Moffitt has had. A key driver of this decision was that Dad is so healthy. Dad set a new goal to go to the gym in their condo once per day. You can imagine with all the treatments, side effects, and tumors that Dad has not been moving and working out as he had before cancer.
Together, Dad and Dr. Ayala signed several consent forms:
- One was consent for the drugs Fludarabine and Melphalan, which are planned for Dad’s conditioning therapy. The purpose of the conditioning therapy is to destroy the cancer cells in Dad’s body. The conditioning therapy starts on the first day Dad is admitted to the hospital, February 4th. In a prior post, I mentioned a Stanford Medicine article that spoke about different conditioning therapies Stanford has been studying for their CTCL stem cell transplant patients. I located a recent presentation of Dr. Youn Kim’s titled “Managing MF and SS with Allogeneic HSCT.” I asked about one conditioning therapy described, in Dr. Kim’s presentation, as a method to reduce GvHD. Dr. Ayala was kind and patient in addressing my inquiry and responding to the printed Stanford presentation slides I put before him on the desk. Dr. Ayala knew of the Stanford research done on that particular conditioning method. It had been published in The New England Journal of Medicine in 2005. He provided his view of the research and shared that Moffitt had a submitted a response to that study. In the end, Dr. Ayala said Dad was getting the best conditioning therapy for his personal situation and that the 2005 Stanford method was not for Dad.
- There were three consents to provide Dad’s data and a blood sample for research purposes within Moffitt and another external organization.
- The last consent was only for patients with European donors. It acknowledges that the European donor may pass Creutzfeldt-Jakob disease, aka Mad Cow disease, onto Dad. At this time there is no test used to identify donors who have Creutzfeldt-Jakob. In recent years, there have been blood and urine tests developed and studied as a reliable screening test. Unfortunately for now, doctors can only confirm the disease with a brain tissue sample. Dr. Ayala reassured Dad by saying that he has never heard of a single transmission of Mad Cow disease in the stem cell transplant community. Dr. Ayala said that it is a “theoretical” risk.
Between now and the admission date of February 4th, Dad continues his radiation therapy with Dr. Montejo. The last radiation treatment is scheduled for January 22nd. Dr. Sokol has squeezed in a second brentuximab vendotin infusion for January 25th.
by Jena | Jan 7, 2016 | Advance Care Planning, Brentuximab Vedotin, Radiation Therapy, Stem Cell Transplant |
Feeling a bit nauseated first thing this morning, Dad started his day at 8:00am at the Moffit Cancer Center’s main campus with a psychological evaluation by Dr. Booth-Jones. Dad claims he “passed.” Dad described several of the activities he had to perform as a part of the evaluation…drawing shapes, selecting alternating colored circles, reading a list of words, repeating sentences read by the psychologist, etc. I actually think Dad found the testing to be interesting and amusing at the same time. I guess we can take heart that Dad is not that loony after all.
All joking aside, I have read that the patient’s mental state before, during and after can impact the outcome of the stem cell transplant. Anxiety and depression have considerable consequences in the months and even years following the transplant. It is best to recognize distress and depression early on through a screening evaluation so that proper psychosocial therapy and pharmacologic medication may be used to help the patient deal with stress before, during and after transplantation. I am appreciative of Dad’s evaluation because Mom and I do not believe Dad would ever admit to being sad or depressed. Dad is constantly trying to remain mentally strong so that Mom won’t worry.
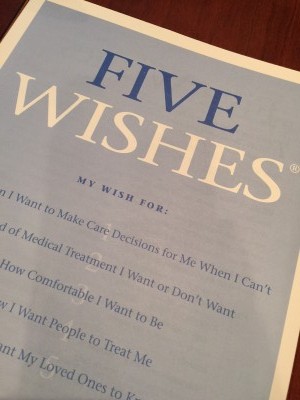
A warm & friendly living will.
At 10:00am, Mom, Dad and I met with Penny, social worker assigned to Dad. We had not met Penny at last week’s meeting with a social worker because Penny was out of the office for the holidays. Penny provided Dad copies of his advance directives (living will and health care surrogate/agent) that he has on file with Moffitt today. I inquired about Five Wishes. I view Five Wishes as a “warm and friendly” living will. Five Wishes also includes the health care agent. Penny said that Dad may use Five Wishes to replace his current one. She also provided another alternative from Project Grace. Penny told us that we could obtain copies of Five Wishes at the Social Worker office rather than order them online from the Five Wishes website. After taking the time to review both, I am recommending that Dad use Five Wishes. I even told Husband that we should update our own advance directives with Five Wishes. I was made aware of Five Wishes through a hospice discussion on the CTCL listserv. (If you haven’t already subscribed to the CTCL listserv and are dealing with CTCL, I highly encourage you to join. It is an online discussion forum with over 1,300 members.)
While riding in the car leaving Moffitt, Dad said we should do some funeral planning. Our family has never been one to avoid or even shy away from end-of-life topics. It probably has a bit to do with personalities. Mom, Dad and I are all type A and appreciate a solid plan…whether is it going on vacation or how one wants to be buried. We LOVE a plan. We keep our conversations about end-of-life light hearted. I got a good giggle when Dad asked me “what do you want at my funeral?” I laughed and reminded him that it is his funeral and that it should be exactly as he wants. Dad then told me that it didn’t matter to him since he “wouldn’t be there” anyway, and it should be what Mom and I want. Classic Dad…ever so selfless.
At 3:30pm, we were at MIP (Moffit Cancer Center at International Plaza). Dad had another dose of radiation to treat the same spots. At 4:30pm, we met with Dr. Montejo, radiation oncology. Dr. Montejo asked how Dad was feeling, and Dad told him about today’s nausea. Dr. Montejo indicated that it could be from the radiation Dad is receiving on his lower spine. That spot is being radiated differently and is “shooting” at Dad from the back and the front. Radiating the lower spine can impact your colon, which may cause nausea. Dr. Montejo had a good look at Dad’s very large tumor on the left/front side of his head..nearly the size of an egg. Dr. Montejo was amazed at how that tumor wasn’t visible when Dad did the radiation simulation two weeks ago. That tumor is open and showing signs of necrosis (visibly black). The good news is that Dr. Montejo indicated that is not infected. Mom was very relieved. Mom takes it personally to be the perfect caregiver by cleaning the open, weeping tumors every evening after Dad showers. She then applies bandages to cover the opens areas. She pads the most sensitive ones hoping the padding will allow Dad to sleep better when he rests his head on his pillow.
Dad doesn’t like to take medication. His whole life, prior to cancer, he would tough it out. He must have thought medication is for wimps. I find I have to tell his doctors that he needs to be encouraged to take pain medication when in pain. Why suffer so much? I had that conversation today with Dr. Montejo. The egg sized tumor is painful. Dr. Montejo convinced Dad to keep a small bottle of OxyContin in his “back pocket” and to take it, if needed. Dr. Montejo feared that Dad might find himself without the ability to get prescription pain medication over the weekend.
Tomorrow is Dad’s last day to do the spot radiation. On Monday, Dad starts eight days of total skin electron therapy (TSET). Dad is not showing any signs of disease on his hands nor feet. This is exciting in that Dad will get to have his hands and feet shielded during the TSET. When Dad did TSET this past summer, I recall Dad having the largest blisters I had ever seen on the tops of his feet. Dad does have a few spots close to his eyes and will have to wear internal eye shields to protect his eyes while radiating around his eyes. If the “egg” and other numerous tumors on his head have not been reduced after those 8 treatments, Dad may receive scalp radiation afterwards.
Tomorrow, Dad will be seen by Dr. Ayala, transplant. Dr. Montejo warned Dad that Dr. Ayala would not like the egg-sized tumor. Dr. Ayala wants Dad to be practically tumor free with no Sézary in his blood before he receives the transplant. I joked with Dad and said that Mom and I could try to cover up the egg with a little concealer makeup…perhaps Dr. Ayala won’t notice.
Page 5 of 6« First«...23456»
 Yesterday, Dad’s second donor, the 19 year old from Germany, was to have his physical evaluation to confirm that he is able to serve as a donor for the stem cell transplant. As of 9:45 p.m. last night, Dad still hadn’t heard. We are a bit frustrated since there has been no communication from Denise, the transplant coordinator, about the donor’s physical evaluation results and a “surprise” appointment for a bone marrow biopsy scheduled for today. Dad attempted to reach Denise via phone and email yesterday with no success.
Yesterday, Dad’s second donor, the 19 year old from Germany, was to have his physical evaluation to confirm that he is able to serve as a donor for the stem cell transplant. As of 9:45 p.m. last night, Dad still hadn’t heard. We are a bit frustrated since there has been no communication from Denise, the transplant coordinator, about the donor’s physical evaluation results and a “surprise” appointment for a bone marrow biopsy scheduled for today. Dad attempted to reach Denise via phone and email yesterday with no success.
 February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs,
February 11th: Repeat of some pre-transplant testing, which expired after 30 days. (CT scans of his sinuses and chest, labs,  The timing of the radiation and systemic treatments Dad has just undergone in January was perfectly aligned for Dad to be admitted this week and receive the stem cells next week. Timing is crucial to increasing the chances of a positive outcome of the transplant. The goal is to have reduced the cancer in Dad’s blood and his skin, as much as possible, at the time the donor’s stem cells are transplanted to Dad.
The timing of the radiation and systemic treatments Dad has just undergone in January was perfectly aligned for Dad to be admitted this week and receive the stem cells next week. Timing is crucial to increasing the chances of a positive outcome of the transplant. The goal is to have reduced the cancer in Dad’s blood and his skin, as much as possible, at the time the donor’s stem cells are transplanted to Dad.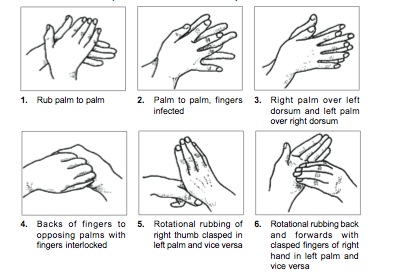

Recent Comments