by Jena | Apr 17, 2016 | Atrial Fibrillation, BK virus, Dialysis, Graft-versus-host-disease (GvHD), Infectious Disease, Meropenem, Minocycline, MRSA, Sepsis, Sirolimus, Stem Cell Transplant, Zosyn |
 Dad was moved to the ICU on the second floor.
Dad was moved to the ICU on the second floor.
Day +13, Friday, April 15th.
WBC: 0.08 k/uL CRITICAL H: 7.4 g/dL LOW P: 18 k/uL LOW Cr: 3.9 HIGH Na+: 148 HIGH
Blood. All three lines (blue, red & white) in Dad’s central line catheter indicated Gram-negative bacteria. Continued minocycline for MRSA and atypical Gram-negative bacteria.
Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed.
Graft versus host disease (GvHD). Dad was unable to take sirolimus since he was restricted from all food and drink.
Mouth & Throat. Dad continued to have pain from mucositis and used magic mouthwash to treat.
Heart. The day before’s echo cardiogram confirmed no heart failure.
Lungs. Dad continued his liquid diet. Again, anytime he drank, he would go into a terrible coughing fit and would require use of an oral suction/vacuum. It was determined that Dad’s epiglottis was not closing properly to prevent food and drink from entering his larynx down to his lungs. The day before’s two chest X-rays showed developing aspiration pneumonia.
Dad had another X-ray taken of his chest. Continued supplemental oxygen. Ordered a nasal feeding tube, but the nurse, who specializes in feeding tube insertions, was unsuccessful in placing Dad’s tube after several attempts.
Abdomen. The day before’s abdomen X-ray showed mild improvement. Imodium was stopped. Dad was switched from Zosyn to meropenem, an ultra-broad spectrum antibiotic.
Kidneys. Nephrology discussed with us the possibility of Dad needing dialysis. The day before’s renal ultrasound showed swelling of Dad’s right kidney due to a possible obstruction. Repeated ultrasound. BK virus was finally confirmed as the source of blood in Dad’s urine. Continued IV fluids and monitored sodium levels. Nephrology also monitored potassium in Dad’s blood and identified Dad as having hypokalemia (deficiency of potassium in the bloodstream). Dad was considered anuric (not passing urine).
Legs. An ultrasound of Dad’s legs, taken the night before, confirmed no blood clots.
by Jena | Apr 17, 2016 | Atrial Fibrillation, Graft-versus-host-disease (GvHD), Infectious Disease, Sepsis, Sirolimus, Stem Cell Transplant, Tobramycin, Vancomycin, Zosyn |
Dad has declined dramatically.
Day +12, Thursday, April 14th.
WBC: <0.01 k/uL CRITICAL H: 7.0 g/dL LOW P: 21 k/uL LOW
Blood. Everyday, Dad’s 3 lumens (blue, red & white) of his central line catheter are tested. The day’s initial blue line test indicated Gram-negative bacteria. Dad was given tobramycin, an antibiotic, to treat. Further testing on the blue line resulted in Dr. Baluch, BMT infectious disease, stopping vancomysin and starting minocycline, another broad spectrum antibiotic.
Dad continued to receive blood support (platelet and blood transfusions & neupogen shots) as needed. Set targets for hemoglobin (H > 8) and platelets (P > 20).
Graft versus host disease (GvHD). Dad continued to take sirolimus to prevent GvHD.
Mouth & Throat. Dad continued to have pain from mucositis. Used magic mouthwash and oxycodone to treat.
Heart. Continued oral Amiodarone to manage atrial fibrillation.
Lungs. Dad had another X-ray of his chest. Continued supplemental oxygen.
Dad was still on a liquid diet. Anytime he drank, he would go into a terrible coughing fit and would require use of an oral suction/vacuum.
Abdomen. Dad continued with Imodium to treat diarrhea. He had another X-ray of his abdomen taken. Dad continued to receive Zosyn as broad spectrum antibiotic.
Kidneys. Creatine (Cr) is the most widely used marker of kidney function in patients undergoing stem cell transplant. Measure of creatine provides an estimation of renal function allows for following trends in renal function. We have learned that acute and chronic kidney disease are common following stem cell transplant and can lead to long-term effects. Stem-cell-transplant-associated kidney injury are often due to a variety of factors including conditioning chemotherapy and sepsis.
Nephrology (kidney doctors) was consulted. Dr. Khimani, inservice Blood & Marrow Transplant (BMT), noted that Dad’s urine output decreased in the prior 24 hours with increased creatine (Cr: 2.3 HIGH). Dad’s sodium also continued to increase (Na: 150 HIGH), which was noted as hypernatremia. Dad continued to receive fluids and have his sodium levels monitored. Dad had a renal ultrasound. Dad was having acute renal failure. He was in septic shock (widespread infection causing organ failure and dangerously low blood pressure) and cardiogenic shock (his heart was unable to pump enough blood to his organs to meet his body’s needs).
Dad was moved to intensive care status. Dr. Baluch, BMT infectious disease, believed that Dad should be transferred out of the BMT unit on the third floor to the intensive care unit (ICU) on the second floor.
by Jena | Apr 17, 2016 | Atrial Fibrillation, BK virus, Epstein-Barr virus (EBV), Folotyn, Ileus, Infectious Disease, Lasix, MRSA, Rituximab, Stem Cell Transplant, Vancomycin, Zosyn |
Catching you up from last Saturday to Wednesday…
Day +7, Saturday, April 9th.
WBC: 0.03 k/uL CRITICAL H: 7.3 g/dL LOW P: 16 k/uL LOW
Dad had continued to go in and out of atrial fibrillation. By the evening, his heart was in normal sinus rhythm (NSR). Dad felt that his abdomen had improved.
Dad noticed increasing throat pain with swallowing. Oral mucositis (mouth sores) can be extremely painful and can result in an inability to eat, speak, or swallow. Last summer, when Dad had received Folotyn (pralatrexate) chemotherapy, he had suffered from oral mucositis. Dad had used magic mouthwash to get some relief. Magic mouthwash is the term given to a solution used to treat oral mucositis.
Abdominal fluid retention improved slightly. Dad had an abdominal X-ray taken.
His diarrhea remained improved. He remained fever free. He remained on 2 L/min oxygen.
MRSA was confirmed on April 6th once Staphylococcus was identified on April 5th.
Day +8, Sunday, April 10th.
WBC: 0.01 k/uL CRITICAL H: 7.3 g/dL LOW P: 13 k/uL LOW
Report from the day before’s abdominal X-ray showed mildly prominent loops in his small intestine, which possibly represented ileus or enteritis. Ileus is the inability of the intestine to contract normally and move waste out of the body. Enteritis is inflammation of the intestine usually accompanied with diarrhea. Dad’s diet was downgraded to clear liquids. His abdominal swelling was improved, yet he continued to receive lasix, a diuretic, to address the fluid retention.
Dad had an X-ray of his chest taken. He was breathing on his own.
Dad switched to an oral amiodarone to manage his atrial fibrillation.
He continued to be monitored for EBV (Epstein-Barr virus), which is more commonly known as mononucleosis or “mono.” Most people will be infected with EBV in their lifetime and will not have any symptoms since it is controlled by a healthy immune system. Yet, when someone has a weakened immune system, the EBV infection can get out of control.
Day +9, Monday, April 11th.
WBC: 0.04 k/uL CRITICAL H: 8.2 g/dL LOW P: 5 k/uL CRIT
The prior day’s chest X-ray suggested inflammation in Dad’s lungs versus fluid overload. Dad’s respiratory culture showed both “gram-positive” and “gram-negative.” These are terms used to classify bacteria into two groups. Usually, gram-positive bacteria are helpful, and gram-negative are the ones that cause illness.
Dad’s atrial fibrillation continued to be addressed with the oral amiodarone. He continued to receive lasix, a diuretic, to address the fluid retention. Dad remained on a clear liquid diet.
The blood in Dad’s urine was suspected to be the BK virus and adenovirus. For most, the BK virus has no consequences since it remains latent, but it can be reactivated during post stem cell transplant when immunosuppressed.
Dad was too tired to work with physical therapy.
Day +10, Tuesday, April 12th.
WBC: 0.02 k/uL CRITICAL H: 8.2 g/dL LOW P: 7 k/uL CRIT
Dad started to choke/cough when eating ice or drinking liquids. Yet, Dad said that his cough had improved and was no longer producing sputum, which is a mixture of saliva and mucus. Respiratory culture from the day before likely indicated MRSA.
Dad’s sodium was high at 148 mmol/L..
Day +11, Wednesday, April 13th.
WBC: 0.01 k/uL CRITICAL H: 8.0 g/dL LOW P: 12 k/uL LOW
Dad continued to be monitored for EBV. Based upon the latest EBV test results, Dr. Ayala, Dad’s primary BMT doctor, was consulted. It was determined that Dad would receive an infusion of rituximab. Rituximab is used to treat EBV post stem cell transplant. Since Dad experienced rigors, fatigue and mild confusion in the morning, the rituximab treatment was postponed.
Dad complained of further pain in his mouth and throat. Dad continued to take oxycodone and magic mouthwash to provide relief from the mucositis. Two X-rays were taken (chest and abdomen). Dad restarted supplemental oxygen.
His cultures indicated MRSA. Dad was started on two new antibiotics, vancomycin and Zosyn (piperacillin/tazobactam). Vancomycin is used to treat infection of the intestines. Zosyn is the combination of two penicillins.
Dad experienced an abnormal heart rate last night, which was resolved with metoprolol. Dad’s atrial fibrillation continued to be addressed with the oral amiodarone. He continued to receive lasix, a diuretic, to address the fluid retention. Dad remained on a clear liquid diet. Dad had a foley catheter placed since he was at a high fall risk. Dad was given Imodium to treat his diarrhea.
Adenovirus was ruled out as the cause of blood in Dad’s urine. BK virus was still a possibility. Set a goal to maintain Dad’s platelets at 20.
Dad’s sodium was high again at 147 mmol/L. Dr. Baluch, BMT infectious disease, noted that Dad’s T. bilirubin was mildly elevated and wanted to monitor trend.
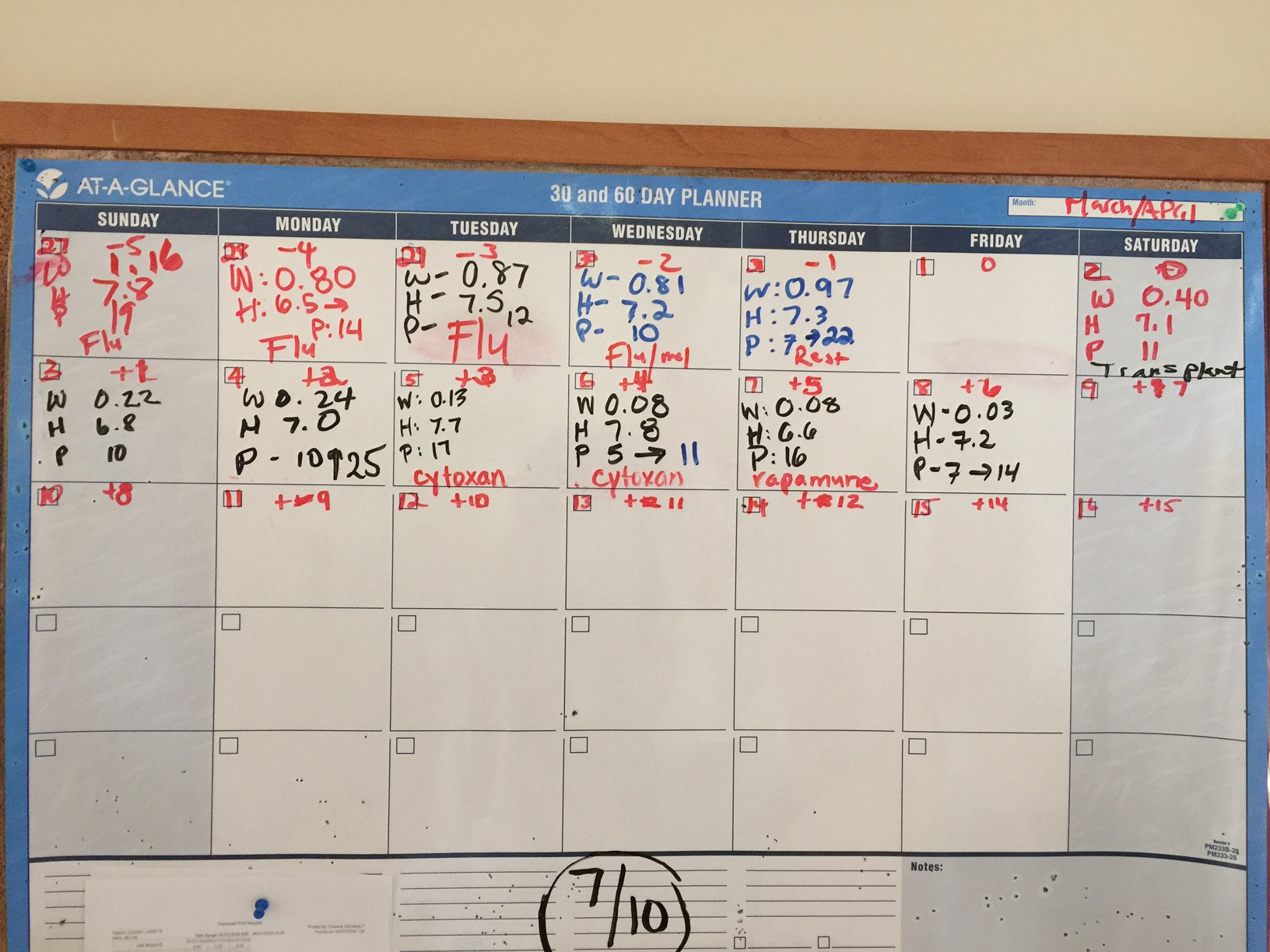
by Jena | Apr 9, 2016 | Atrial Fibrillation, Cyclophosphamide, Fludarabine, Graft-versus-host-disease (GvHD), Ileus, Infectious Disease, Melphalan, Sirolimus, Stem Cell Transplant |
Today is Day +7. Dad is doing fairly well considering he is in week two, which is one of the worst weeks that stem cell transplant patients endure. He has experienced a variety of issues as expected.
Three blood counts are tracked daily…white blood cell (WBC), hemoglobin (H), and platelets (P). Patients feel the worst as their WBC count plummets to zero, which occurs during week 2.
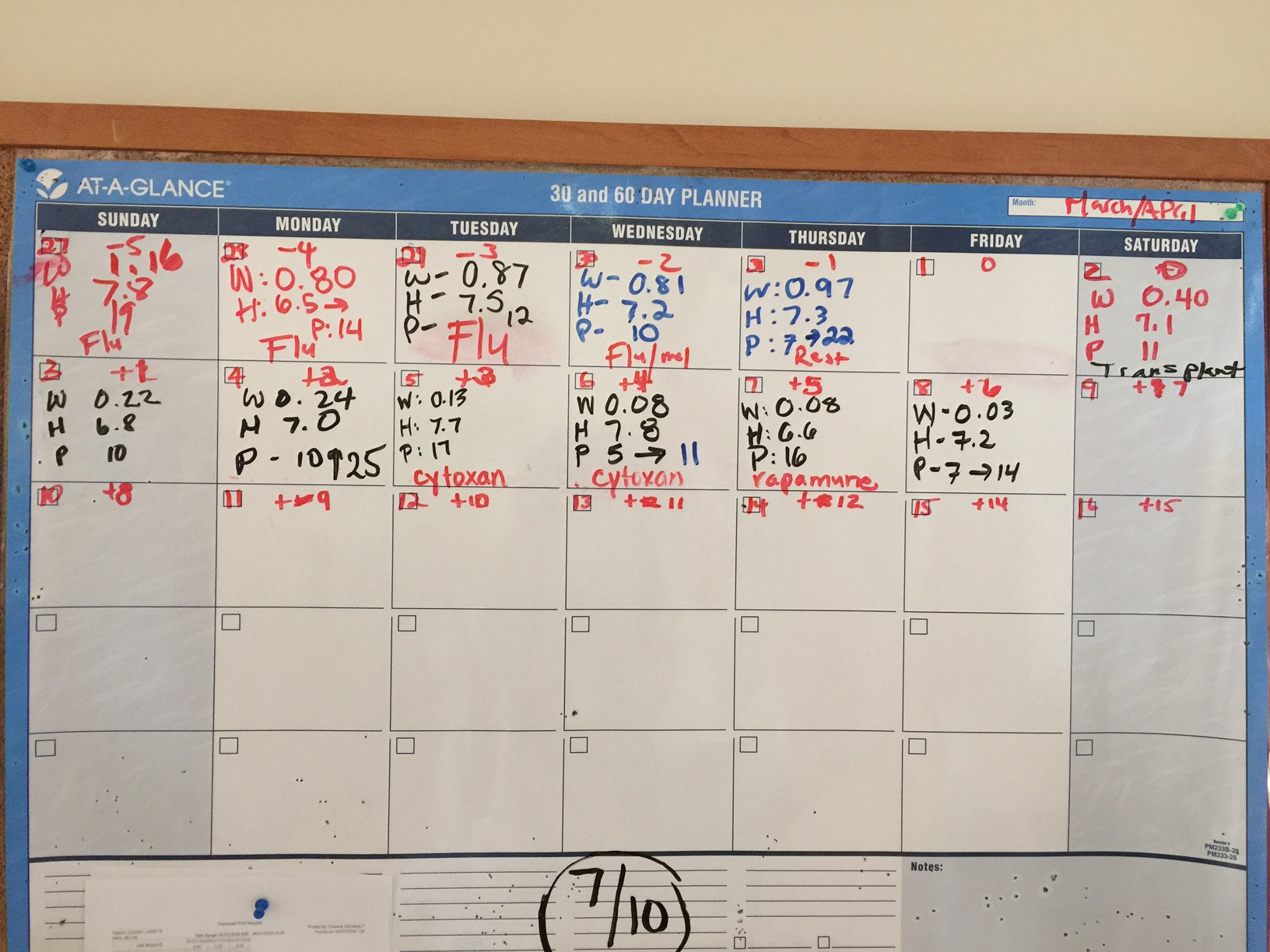
Here’s a recap since I last posted on Day +2.
Day +3, Tuesday, April 5th.
WBC: 0.13 k/uL CRITICAL H: 7.7 g/dL LOW P: 17 k/uL LOW
Dad was fatigued. He complained that he did not sleep well. He was restless. During the day, Dad was napping frequently to catch up on his missed sleep. Dad continued to have diarrhea, which was attributed to the toxicity of the melphalan (one of his two conditioing chemotherapies received on Day -2). Dad was given Imodium to address the diarrhea.
Dad also received his first of two doses of Cytoxin (cyclophosphamide). Post-transplantation cyclophosphamide (Day +3) prevents acute and chronic GvHD (graft-versus-host-disease).
Dad showed no signs of tremors. Doctors believed it was due to toxicity from the fludarabine chemotherapy, which Dad received on Day – 5 through Day – 2.
Day +4, Wednesday, April 6th.
WBC: 0.08 k/uL CRITICAL H: 7.3 g/dL LOW P: 11 k/uL LOW
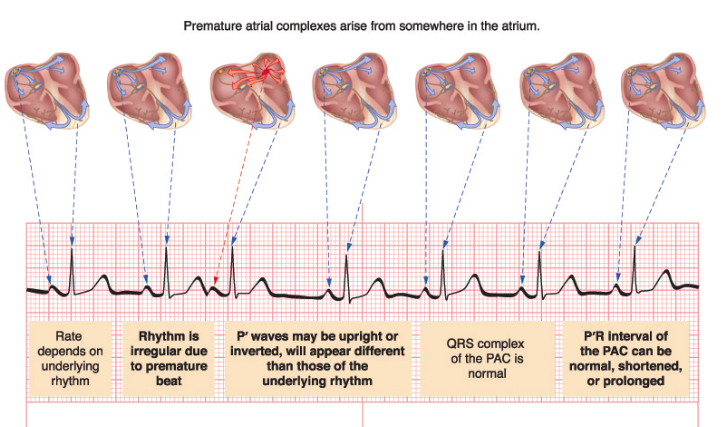
Overnight, Dad had spiked a fever of 101.9 and experienced tachycardia (abnormally rapid heart rate). His heart rate went as high as 175 bpm. He was treated with Lopressor (metoprolol) to help abate the tachycardia. Cardiology was consulted, and two electrocardiograms (ECG) were done (12:43 a.m. and 9:14 a.m.). Both ECGs returned similar results of sinus tachycardia (sinus rhythm with an elevated rated of impulses) with premature atrial complexes (APC).
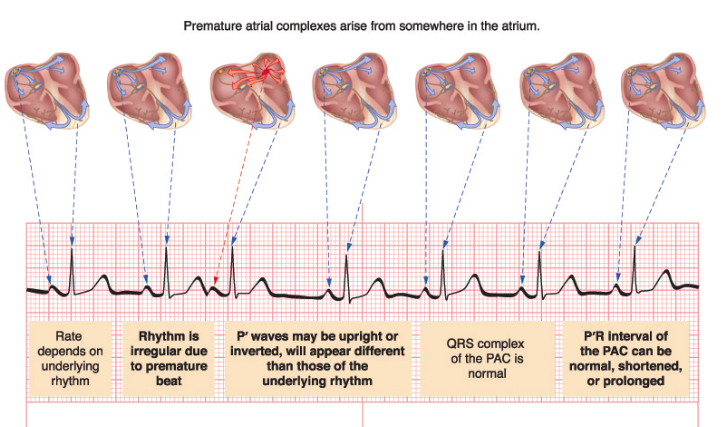
Later mid-afternoon, Dad had an echocardiogram. Dr. Fradley, cardiologist, assessed Dad and concluded that Dad is asymptomatic during these short-lived episodes. He expected that Dad would have arrhythmia due to Dad’s melphalan chemotherapy, which Dad received on Day -2. 12% of patients develop atrial fibrillation from melphalan. He recommended rate control with metoprolol.
Dad had an episode of decreased oxygen saturations. An arterial blood gas (ABG) test was run to measure the acidity (pH) and the levels of oxygen and carbon dioxide in his blood. Dad was put on 3 L/min of oxygen via a nasal cannula.
Dad was also started on Vancomycin via IV to address possible infection in his intestines. Dad continued to have diarrhea and was fatigued. Dad started to note pain in his throat.
Dad was showing signs of fluid retention. He was given two doses of lasix. Dad was having to urinate constantly.
His chest X-ray showed no evidence of pneumonia.
Dad received a platelet transfusion and his second and final dose of Cytoxin (cyclophosphamide).
Day +5, Thursday, April 7th.
WBC: 0.08 k/uL CRITICAL H: 6.6 g/dL LOW P: 16 k/uL LOW
Overnight, Dad went into atrial fibrillation. He was initially given metoprolol via IV. He was then given diltiazem. After Dad experienced low blood pressure and uncontrolled heart rate with diltiazem, he was switched to amiodarone plus digoxin. Dad had another ECG at 8:30 a.m. It was abnormal confirming the atrial fibrillation. Dr. Robinson, cardiology, believed the atrial fibrillation was due to the melphalan chemotherapy, which Dad received on Day -2.
Patients with atrial fibrillation are at greater risk of deep vein thrombosis (DVT). Yet, Dad cannot take an anticoagulant since he is thrombocytopenic (low platetet count).
Dad continued to have diarrhea. He continued to receive Imodium to address. He also continued to receive lasix to address his fluid retention.
Dad complained of tickling of his throat. He was coughing after eating and drinking, thus speech therapy gave him an evaluation. Speech therapy recommended that Dad eat and drink only when sitting up completely. He continued to receive 2 L/min of oxygen.
As planned, Dad was given Rapamune (sirolimus) orally as a prophylaxis against GvHD. He will take sirolimus for 28 days.
Day +6, Friday, April 8th.
WBC: 0.03 k/uL CRITICAL H: 7.2 g/dL LOW P: 14 k/uL LOW
Dad said he received the best night’s sleep he has had in two years. I found that to be quite incredible. The good news was that he was no longer having diarrhea. Dad said his mouth was dry and continued to have discomfort in his throat.
Dad received a platelet transfusion to raise his count from 7 to 14 k/uL.
Late in the morning, Dad finally was up and walking after two to three days of remaining in bed. I brought in a small megaphone for Mom and the physical therapist (PT) to use to encourage Dad to move more. George, the PT, was amused. He had Dad out of bed and moving down the hall with an entourage. Dad was using a walker, and George had a firm grip of the “belt” around Dad’s waist in case Dad fell or collapsed. Dad will have to work himself back up to walking 2 miles a day.


Italian ice is a part of Dad’s new, liquid diet.
Dad had his abdomen X-rayed since it continued to look enlarged. X-ray showed air levels concerning for ileus or obstruction. Patients can develop gastrointestinal (GI) ulcers, vomiting and dairrhea from melphalan. This nasty chemotherapy strips the mucosa of the GI tract. Severe cases can develop ileus or even perforation of the bowel wall. Dad was prescribed Flagyl (metronidazole) as an antibiotic for his abdomen. He was put on a clear liquid diet in order to give his intestines a rest.
Dr. Baluch, BMT (blood & marrow transplant) infectious disease, indicated that Dad would stop receiving vancomycin after today, if he had no more fevers nor positive cultures.
Dad’s urine showed a small amount of blood, but not enough to cause alarm. Another urine analysis to be conducted in one to two days to monitor.
Dad continued to receive lasix to address his fluid retention. He also continued to receive 2 L/min of oxygen.
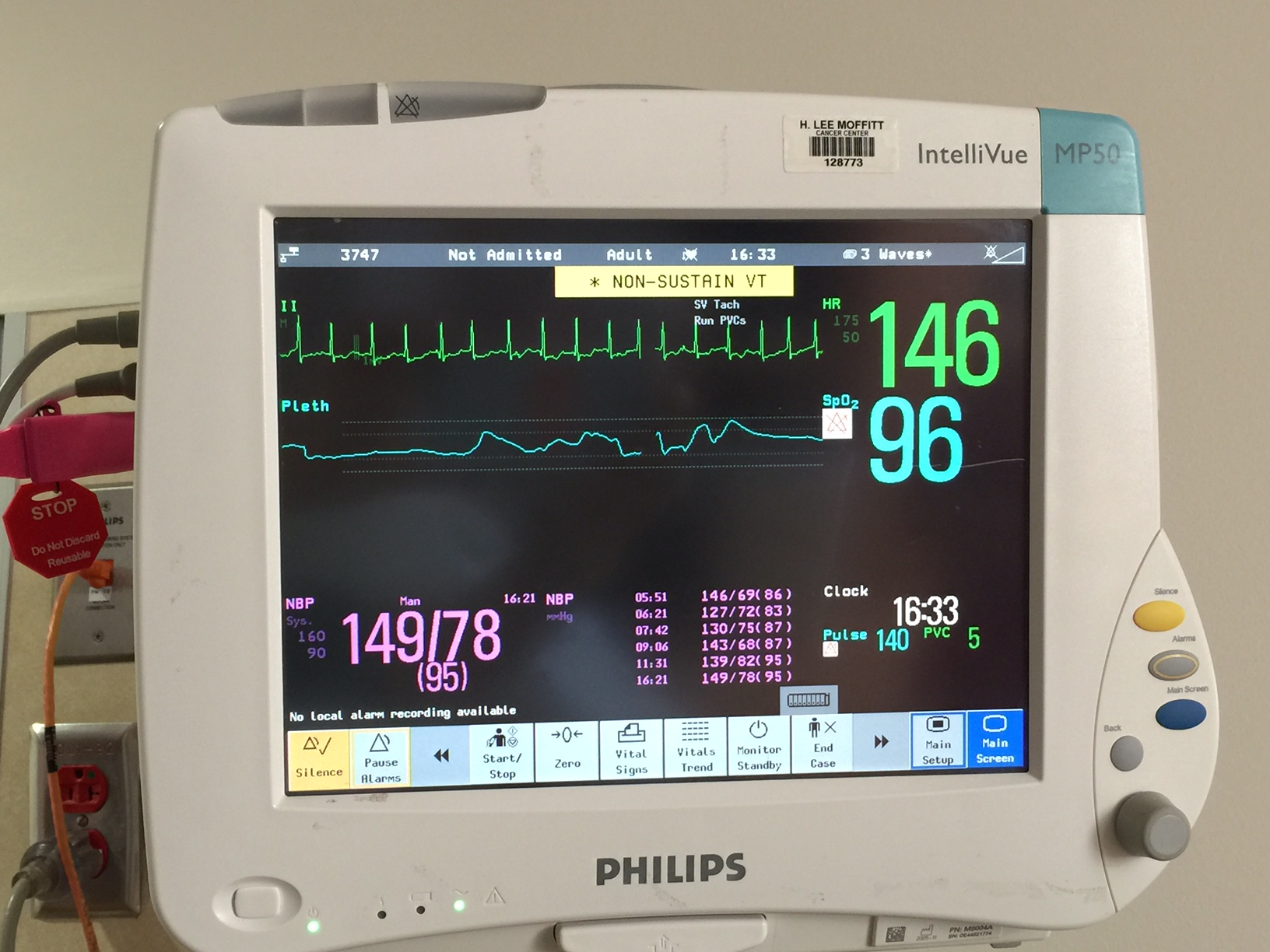
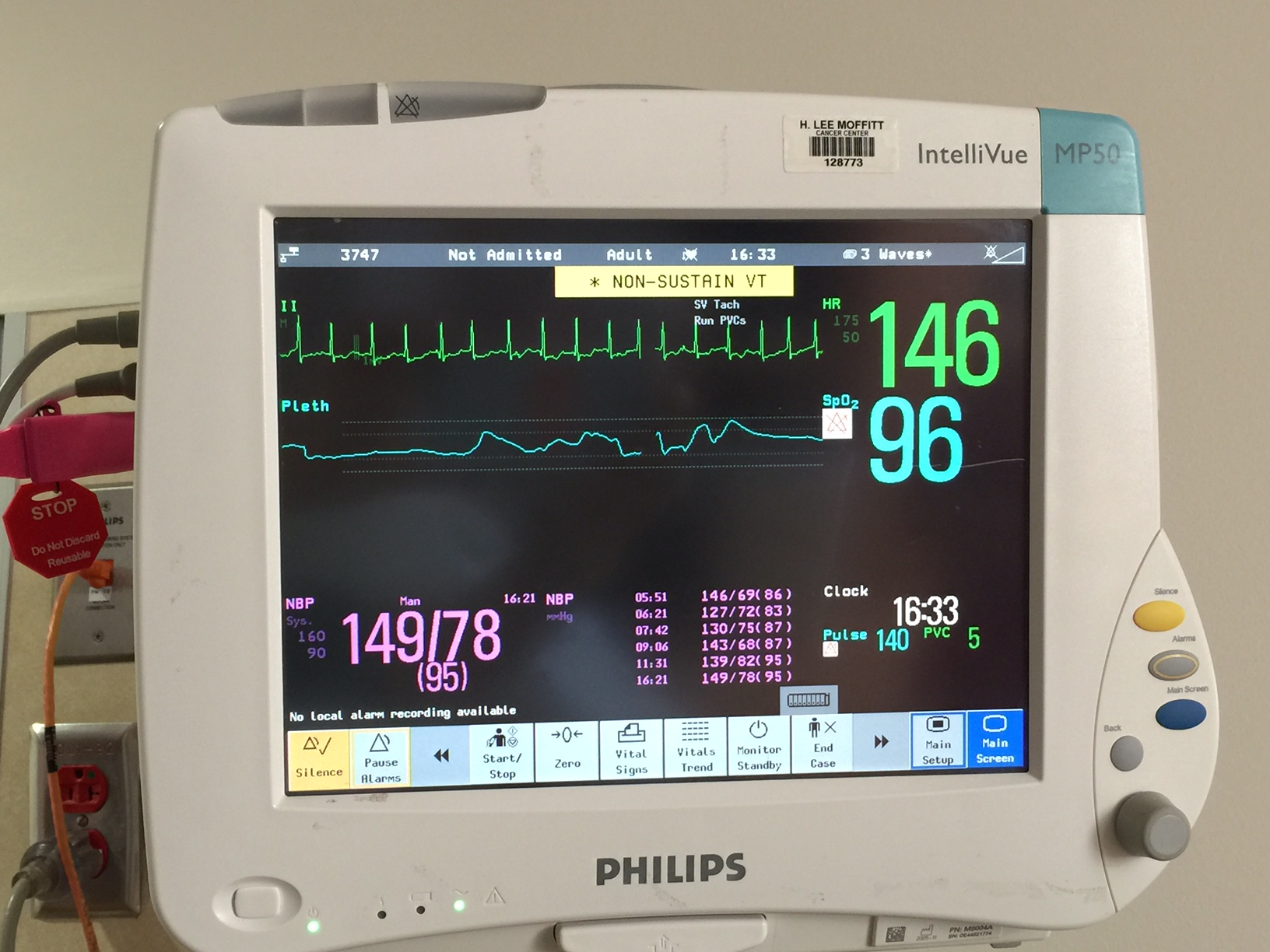
Dad’s heart and oxygen monitor showing 146 bpm.
Late morning, the cardiologist, Dr. Robinson, was thinking that Dad’s heart was improving and had sustained a normal sinus rhythm (NSR). Dr. Robinson had begun to plan how Dad’s heart medications would begin to taper. Unfortunately, Dad’s heart rate was racing again in the afternoon.
by Jena | Apr 4, 2016 | Cytomegalovirus (CMV), Graft-versus-host-disease (GvHD), Graft-versus-tumor (GvT), Sirolimus, Stem Cell Transplant |
Day +2, Monday, April 4th. Our two week spring break is over. Husband left the house at 4:30 a.m. to catch a flight to Ohio for work. Daughter was sunny and lively this morning despite still having coughing fits. She has one more day of antibiotics to address her bronchitis. Son stayed home from school and remained in bed due to his cold.
After dropping Daughter off at school at 7:30 a.m., I checked in with Mom and Dad. Mom was still in bed on the sleeper sofa. The lights were off in Dad’s room. Mom said that they had a rough night. Dad was now having diarrhea. After a minute or so on the phone with Mom, Dad needed to go to the bathroom. Alarms were sounding in his room. Dad was no longer allowed to get out of bed on his own. He was deemed too weak. I could hear the nurse, over Dad’s room’s speaker, telling my Dad to stay in bed until someone arrived to assist him. Needless to say, Mom and I ended our early morning call.
Dad FaceTimed me at 2:00 p.m. Dad was much improved. His eyes were bright and happy. He spoke with more vigor. The volume of stem cells and related fluids during the transplant infusion was rather large. Dad received 800mL on Saturday evening. Leslie, daytime nurse, said that transplant infusion volumes can be as small as a couple hundred mL to as large as 1 L (1000 mL). It is believed that the large volume of donor “fluids” received by Dad was the cause of his nausea and diarrhea. His body was unhappy about so much foreign substance.
I learned that Dad had a fever yesterday in addition to the nausea. It spiked at 101. This triggered the normal fever protocol to have a chest X-ray taken. Results from yesterday’s X-ray depict some spots. These spots have triggered a CT scan to be ordered. Dad should have the scan done today. Mom and Dad hope that Dad doesn’t require another bronchoalveolar lavage.
Dad mentioned that they rotated inservice BMT (blood & marrow transplant) doctors today. Dr. Khimani was now the inservice BMT.
Graft-versus-host-disease (GvHD) remains a major cause of morbidity and mortality after allogeneic transplantation, which is the type Dad received on Saturday. The older the recipient, the higher the risk for GvHD. We chatted with Leslie about Dad’s upcoming sirolimus medication on Day +5. Sirolimus prevents GvHD. Mom asked Leslie to print out hardcopy information containing facts, side effects, etc. about the drug. Mom studies all the drugs in detail.
Measures, previously developed that had significantly reduced GvHD, had been frequently associated with an increased risk of relapse. GvHD and graft-versus-tumor (GvT) effects are tightly linked, and balance between both reactions is difficult to achieve. The drug sirolimus has immunosuppresive, antitumor, and antiviral properties. Sirolimus’ unique properties give it an advantage over other immunosuppressive agents. It promotes GvT by allowing the new (donor’s) T cells to attack Dad’s remaining cancer cells, and it inhibits antigen presentation of by Dad’s antigen presenting cells (APCs). Recognition of Dad’s antigen by his new (donor’s) T cells commonly results in GvHD. Sirolimus also exerts antiviral actions, especially against the cytomegalovirus (CMV).
When FaceTiming with Dad at 5:00 p.m., Mom was making preparations to have Dad shower. Dad wanted to be showered for the evening before getting his CT scan at 6:30 p.m.
 Dad was moved to the ICU on the second floor.
Dad was moved to the ICU on the second floor.


Recent Comments