Dad’s Many Ducks


Yesterday, after Dad got home from Moffitt, Mom called me at 4:30 p.m. to say that Dad had a fever, 100.4, and was experiencing some chills. Dad spoke to the Moffitt nurse via phone. The nurse told Dad to take Benadryl since she believed his fever was a reaction to his platelet transfusion. Dad traditionally takes pre-medications to prevent reactions, but for some reason, Dad didn’t take any prior to his platelet transfusion yesterday.
Yesterday evening, I spoke to Mom and Dad at 6:00 p.m. asking how Dad was feeling after taking the Benadryl. He indicated that he was improving.
On the way home from dropping the kids off at school this morning, Thursday, I called to check on Dad. Unbeknownst to me, I learned that Dad had checked into the hospital at Moffitt at 1:30 a.m.
Last night, Dad had taken another dose of Benadryl at 10:00 p.m. Dad had then taken his temperature multiple times at 11:30 p.m. Results were 98.4, 100.2 and 101.2. They had been concerned and had called the Moffitt night nurse again. Dad was instructed to come into Moffitt in the middle of the night.
I wasn’t happy that Mom and Dad sneaked off, in the middle of the night, to Moffit without my knowledge.
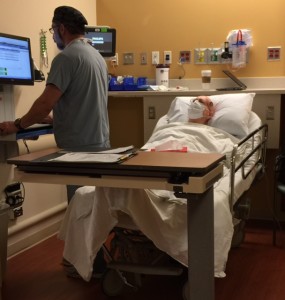
Upon arrival to Moffitt last night, Dad had numerous vials of blood taken and a chest X-ray, using a portable machine. Around 4:30 a.m., he has his nose swabbed. I arrived around 10:00 a.m. Shortly thereafter, Dr. Ayala, transplant doctor, came in with four others. They were dressed in their yellow, disposable gowns, bright blue gloves, and yellow, duck masks. Dr. Ayala gave Dad a brief physical exam. He wanted to know if Dad had been experiencing anything more than a fever. Dad said he hadn’t. Dr. Ayala also checked Dad’s mouth. No sign of redness. Dr. Ayala wanted a better look at Dad’s lungs since the portable X-ray was a bit cloudy and was showing a couple of patches. Dr. Ayala ordered another (better) X-ray. As the team of doctors were leaving Dad’s room, Dr. Ayala teased Dad about showing up too early for his Sunday, inpatient check-in for his stem cell transplant and said “…no more fun and games.”
The better X-ray showed spots in Dad’s right lung. Dr. Baluch, infectious disease, then ordered a CT scan of Dad’s lungs. Later, Harmony, physician assistant (PA), came by with the initial results of the CT scan. Dr. Baluch is concerned about two spots, which look like fungal pneumonia. Harmony pulled up Dad’s CT scans from February 11th and today. By comparing the two, it was evident that the two spots are new on today’s CT scan. Harmony said that fungal pneumonia is uncommon and mostly seen in patients who are neutropenic and could take weeks to months to eliminate.

Bronchoalveolar lavage (BAL)
Dr. Chan, pulmonary, came by to learn about Dad’s history and current symptoms. She described a bronchoalveolar lavage (BAL), a diagnostic procedure, where fluid is introduced into the terminal bronchioles and then recollected for analysis. BAL aims to establish a diagnosis to find out if an infection is present. Later, Dr. Chan consulted with Dr. Walsh, also in pulmonary. The plan is for Dad to stay at Moffitt tonight and to do the BAL in the morning.
We are still waiting to meet with Dr. Baluch, infectious disease, in order to get her view of how the fungal pneumonia impacts Dad’s stem cell transplant schedule. We know that the probability is high that Dad will not start his stem cell transplant preparations as an inpatient on Sunday as we were hoping. Mom is extremely disappointed.
As I was typing this post, Mom was assisting Dad with his shower. Mom stepped out of the bathroom, momentarily, to get Dad a fresh pair of pajamas. Then, we heard what sounded like Dad falling in the shower. Fortunately, he caught himself by pulling on the shower alarm. In an instant, Dad’s nurse, technician, and another gentleman ran to Dad’s room. Thank goodness it was a false alarm! I reminded Dad that he is at severe risk of dying from a brain bleed if he were to fall and hit his head. His platelets are so low that he has little ability to clot.
Dad, no more fun & games…especially in the shower.
 This past week has been mostly filled with trips to Moffitt for Dad to get his central line catheter flushed daily and to receive blood support.
This past week has been mostly filled with trips to Moffitt for Dad to get his central line catheter flushed daily and to receive blood support.
Saturday, February 20: Dad had to go to the main campus of the Moffitt Cancer Center since the Moffitt Cancer Center at International Plaza (MIP) is only open on weekdays. Dad’s dressing for his central line catheter was changed. His line was flushed.
Sunday, February 21: Back at the main campus of Moffitt again, Dad had his central line catheter flushed.
Monday, February 22: At Moffit Cancer Center at International Plaza (MIP), Dad had his central line catheter flushed and a blood draw to check his counts. All counts (white blood cells, platelets and hemoglobin) came back low.
Tuesday, February 23: Dad returned to MIP for his daily central line catheter flush. He received two bags of blood via transfusion to boost his hemoglobin level.
Wednesday, February 24: Dad went to the main campus of the Moffitt Cancer Center. He met with Denise, the transplant coordinator, and she shared good news. The 19 year old donor was able to reschedule so that Dad can be admitted this Sunday, February 28th to begin his stem cell transplant process. We are very happy! Dad also had his daily central line catheter flushed and received a platelet transfusion.
At 8:00 a.m., Dad had his blood counts checked to determine whether or not he needed another platelet transfusion to get his platelet count above 50 (50,000/mcL of blood). 50 is required for the medical procedure to place Dad’s new central line catheter. Dad’s platelet count came back at 64. Thus, no need for a platelet transfusion this morning. It was important for Dad to have enough platelets in order to clot, as needed for the procedure.
Dad getting ready for his central line catheter procedure.
At 10:00 a.m., Dad was prepped for his central line catheter procedure in the outpatient surgery department. Two small incisions were made in Dad’s upper right chest. One incision was made near his neck, and the second was made a little lower to insert the catheter into the proper place. The catheter was “tunneled” under his skin. He received some stitches in his chest close to the catheter exit. These stitches will be removed in 21 days when his skin has healed around the catheter. The procedure took about 45 minutes with an additional 30 minutes for recovery.
When Mom and I went to see Dad in recovery, he was happily drinking an orange Gatorade. He hadn’t been able to eat nor drink since midnight the day before. We discussed plans to eat lunch. We were determined not to eat in the Moffitt cafeteria since Dad, along with Mom and I, would be eating this food for the next month. Dad was craving pizza. Mom was adamant that Dad not dine in a restaurant for fear of picking up an illness. Thus, we agreed upon take-out. Dad seems to enjoy Little Caesar’s HOT-N-READY DEEP! DEEP! Dish pepperoni pizza. I am not a pizza fan, but I want Dad to enjoy his last few meals “outside” of Moffitt. It should be all about what he wants to eat.
At 12:30 p.m., we returned to the Blood & Marrow Treatment (BMT) Center to learn about post-insertion care. Dad may have some discomfort in his shoulder and chest area over the next few days. The physician’s assistant (PA) recommended 1,000 mg of Tylenol to relieve any discomfort. They provided ice packs for Dad to apply to the catheter site 20 minutes at a time, every hour, as needed for the first 24 – 48 hours. Dad is to expect a small amount of blood and bruising around the exit site. He cannot shower for 48 hours.
We did find it odd that the BMT nurse had to remove Dad’s PICC line since the surgery team did not remove it during Dad’s central line catheter procedure. We had been under the impression that it would occur during the surgery. This was even discussed with the doctor 20 minutes prior to the procedure.

Nurse removing Dad’s PICC line.
The nurse indicated that removing a PICC line was rather commonplace in the BMT treatment center. The nurse removed the dressing on and around the PICC and pulled the line right out of Dad’s left arm. The amount of line that came out of Dad’s arm was incredible. How could all that line be inside of him? The nurse felt bad since a couple drops of blood fell onto his shirt. She worked hard to remove the blood stain.
As we were getting our final questions answered, Dad happened to mention to the nurse that he has had a slight sore throat the past three days. Mom and I were unaware of this slight sore throat. Well, that sounded the alarms! The nurse went to speak to the PA. Dad had his nose and throat swabbed to check for infection. The PA looked at Dad’s throat and said it looked like strep throat. The PA consulted with two other PAs, who also examined Dad’s throat, and agreed that it looked like strep. The PAs were puzzled since Dad’s throat was only slightly sore. They ran a rapid-strep test, which came back negative. For now, the initial diagnosis is rhino-virus (the common cold) and potentially something fungal. Dad was prescribed two medications. The swab results won’t be back from the lab for a few days to provide a more definitive diagnosis.
The PA consulted with Dr. Ayala. The bad news is that Dr. Ayala has postponed Dad’s stem cell transplant. He won’t be admitted on Sunday. This is very upsetting for Mom. Dad is now scheduled to see Dr. Ayala on Wednesday, February 24th.
We are on the stem cell transplant roller coaster.
This morning Dad had his third bone marrow biopsy and received two bags of platelets in anticipation of the procedure to place his central line catheter tomorrow, Friday, February 19th.
At 1:00 p.m., we met with two different nurses, not Denise, and Dr. Ayala. First, we learned that the 19 year old donor passed the physical examination. Excellent.
 Next, Dr. Ayala examined Dad and confirmed that Dad is ready for the transplant and that his disease
Next, Dr. Ayala examined Dad and confirmed that Dad is ready for the transplant and that his disease
is minimized as much as possible. Dr. Ayala reminded us that every transplant is different and that there will be bumps along the way. He stressed the importance for Dad to stay very active physically and mentally. Dad bragged to the doctor that he was in the gym earlier in the week for 45 minutes with 20 minutes on the stationary bike.
Dr. Ayala reviewed the risks of the transplant again. CTCL patients are at a high risk of skin infection since CTCL is a skin related cancer. He also discussed graft versus host (GvH), and he reminded us that Dad’s chance of death is 25-30%, which is higher than the traditional CTCL patient due to Dad’s age. At 75.9 years old, Dad will be the oldest patient to ever receive a stem cell transplant at the Moffitt Cancer Center. Wow! Doctors seem to believe that Dad’s body is closer to that of a healthy 55 year old. The medical staff continue to be amazed with Dad’s positive demeanor and “can do” attitude. They also recognize the outstanding support Mom provides non-stop daily. I know that these are key drivers in Dad being a candidate for a stem cell transplant. Dad is raising the “age” bar.
As we discussed the risk of death, Dr. Ayala said he would be honest and forthright about Dad’s condition. Dr. Ayala shared his view about not using life support. Dad reviewed his advance directive, now using Five Wishes, with Dr. Ayala. Dad made it clear as to when he would want to be resuscitated and when he would not. I inquired about ensuring that Dr. Ayala would indicate the best time to transition to hospice.
Days are named and tracked based upon the actual day Dad is to be infused with the donor’s stem cells. The days leading up to that day are noted as “negative” while the days after are noted as “positive.”
The plan for Sunday, February 21 (aka DAY -5), is for Dad to call at 10:00 a.m. to see if a bed is available. If so, we go to Moffitt and check Dad in as an inpatient. If no bed is available yet, Dad will go to the Blood and Marrow Transplant clinic, also at the Moffitt Cancer Center, for blood work and prep for his first of four days of chemotherapy, fludarabine, to begin Sunday evening. The assumption is that a bed will eventually be available that same day.
Last, we spent a fair amount of time with two pharmacists, Bryan, a pharmacist resident, and Amy. All of Dad’s current and future medications were reviewed in great detail. We discussed the two chemotherapy drugs, fludarabine and melphalan, to be given during the first four days of Dad being an inpatient. Melphalan is a drug, which may cause Dad mucositis. Last year, Dad experienced severe mucositis of the mouth as a terribly painful side effect of FOLOTYN, another chemotherapy drug. He was living on milkshakes and Boost for one to two weeks.
The pharmacists said that Dad will be infused with the donor’s stem cells as soon as they arrive…even in the middle of the night, which is the famous DAY 0.
We also discussed what will be done to prevent GvH. The donor’s cells could attack Dad’s skin, GI tract and liver. The first method of prevention is through intravenous cyclophosphamide on DAY +4 & DAY +5. This drug can delay the time for the cells to engraft. Cyclophosphamide does not harm the donor’s stem cells. It spares the good T-cells (regulatory T-cells) and knocks out the harmful T-cells. The second method of GvH prevention is sirolimus, starting on DAY +5.
Also starting on DAY +5 is a daily neupogen shot to accelerate the recovery of the new stem cells. The daily shots of neupogen will be given until Dad achieves a neutrophil count of 1,500/mm3 of blood.
Recent Comments